Your sacroiliac (SI) joints connect your spine to your pelvis, and can cause lower back pain and other symptoms when inflamed or injured. Sacroiliac joint pain is estimated to be the cause of 15-30% of all lower back pain episodes [1]. We explore what SI joint pain is, what the symptoms are, and the treatment available on the NHS.
Treatment may include medication, physiotherapy, injections and surgery. However, there can be a long wait for treatment on the NHS, during which your symptoms may get worse. For that reason, many people opt for private treatment, such as the rapid-access services offered by Harley Street Specialist Hospital.
What is sacroiliac joint pain?
Your SI joints are the joints where the lower part of your spine (sacrum) connects to your pelvis. You have two SI joints, one on each side.
These joints help to stabilise and support your spine. They also absorb impact during activities like walking and lifting.
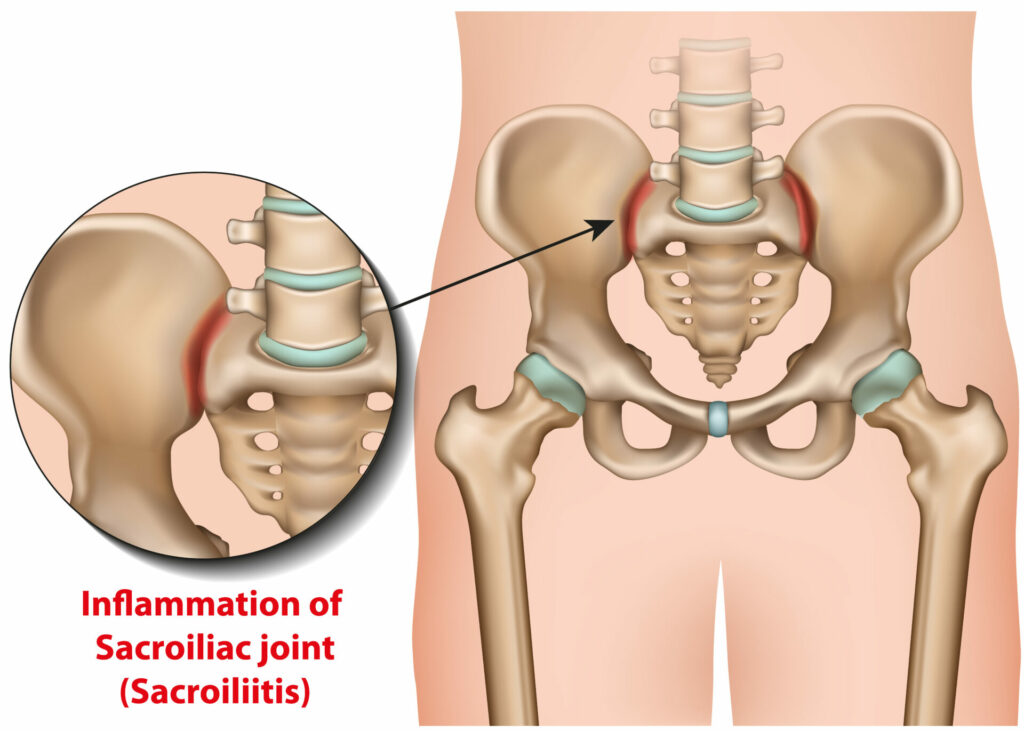
The SI joints are supported by ligaments and muscles, which only allow a very small amount of movement within the joints. They are synovial joints, meaning a type of joint where two bones move against each other. Like most synovial joints, your SI joints are filled with fluid.
SI joint pain can range from mild to severe, depending on the cause of your pain and to what extent it’s impacting your joints. SI joint pain may also be described as SI joint syndrome, SI joint strain, SI joint inflammation, sacroiliitis and SI joint dysfunction.
SI joint pain can be acute or chronic. Acute pain occurs suddenly and usually resolves within a few days or weeks. Chronic pain may come on suddenly or slowly over time and lasts for more than 3 months. It may be a constant pain or only felt with certain activities.
Symptoms of SI joint pain
You will usually feel pain in your lower back or buttocks, which can radiate to your groin, thigh or hip. Radiating pain means pain that migrates from where it started and spreads to other parts of your body.
You may also feel numbness, tingling or weakness in your leg. Although SI joint pain usually occurs on one side, it can occur on both sides at the same time.
What else could be causing your pain?
Lower back pain is the main symptom of SI joint dysfunction. However, there are many other potential causes of lower back pain. These include:
- Arthritis of the spine – This is wear and tear to the joints of your lower back.
- Herniated disc – A disc between the bones of the spine moves out of place and can push on a nerve, causing pain.
- Sciatica – This is irritation and inflammation of the sciatic nerve, often caused by a herniated disc.
- Muscle or ligament injuries – These often occur when moving suddenly or doing a movement you’re not used to.
- Spinal fracture – A fracture is a broken bone, that usually occurs in the lower back as a result of an accident or injury.
- Spinal stenosis – This is narrowing of one or more spaces within your spinal canal.
How is SI joint pain diagnosed?
Before it can be treated, SI joint pain must be diagnosed correctly. Your doctor or physiotherapist will complete a full medical exam, including a detailed history of your pain and symptoms.
The physical exam may include specific tests, and you will be assessed in different positions to see what brings on your pain. They may manually move your joints or feel your lower back for tenderness.
Your doctor may arrange diagnostic imaging, such as an X-ray or MRI scan. This will help to diagnose SI joint pain and identify any other lower back and spine conditions that may be causing your symptoms.
SI joint injections are often used for treatment but can also be used for diagnosis. The clinician injects anaesthetic and corticosteroid medication into your SI joint, often using imaging to guide the injection.
Your pain level is noted before the injection, 30 minutes after, and monitored over the following week. If your pain levels decrease significantly following the injection, a diagnosis of SI joint pain is made. If your pain levels don’t change at all, the SI joint is unlikely to be the cause of your pain.
What treatment for sacroiliac joint pain is available on the NHS?
The NHS can treat SI joint pain with medication, injections, physiotherapy and surgery. Let’s look at each of these treatment options in more detail.
Pain medication
The type of medication selected will depend on the cause of your SI joint pain. Your doctor may prescribe nonsteroidal anti-inflammatory drugs (NSAIDs) if inflammation is worsening your SI joint pain. These include over-the-counter medications like ibuprofen and stronger prescription medications.
You may also experience painful muscle spasms with your SI joint pain. Your doctor may prescribe muscle relaxants for these spasms, such as diazepam.

Biologics
Biologic medications treat autoimmune conditions like rheumatoid arthritis, which can affect the sacroiliac joint. Autoimmune conditions are when your body’s immune system mistakenly attacks healthy tissue in your body.
These medicines work by blocking certain proteins or chemical pathways linked to inflammation. This can slow down or stop inflammation, preventing damage to your joints. However, current research into the use of biologics for SI joint pain is limited to people who have been clinically diagnosed with an autoimmune condition and have tried and failed other types of therapy [2].
Physiotherapy
Physiotherapy and exercise are usually one of the first lines of treatment for SI joint pain. Research shows that physiotherapy, particularly exercise therapy and joint manipulation, is highly effective at treating SI joint pain [3].
Physiotherapy exercises aim to restore normal function to the SI joint by strengthening muscles that support the joint. These are known as stabilisation exercises and have been shown to improve SI joint pain and dysfunction [3]. Simple exercises for back pain also aim to stretch and relax excessively tight muscles around the joint that are limiting normal movement.
Research shows that in people with SI joint pain, the gluteus (buttock) muscles on the affected side and the latissimus dorsi (a large muscle of the mid and lower back) on the unaffected side are usually overactive. Correcting this imbalance in muscle activity through stretching and strengthening improves SI joint pain [4], but requires the support of a physiotherapist.
Another aspect of physiotherapy is manual therapy, where the therapist passively moves your joints at varying levels of speed and pressure. Joint manipulation is a type of manual therapy that involves sudden, high-speed thrusts of movement to a joint. It is a highly skilled treatment and should only be attempted by trained physiotherapists.
Research shows that joint manipulation is successful at relieving SI joint pain, and some studies indicate it may be more effective than exercise as a treatment method [5, 6]. However, other research suggests that both exercise and manipulation are equally effective [3].
Sacroiliac joint injections
Injections can be used to diagnose and treat SI joint pain. These injections may be intra-articular (within the SI joint) or periarticular (around the SI joint). There’s research to suggest that periarticular SI joint injections may provide better pain relief [7].
Steroid injections
There are different types of injections offered on the NHS that may improve SI joint pain. The most common type is a steroid injection, in which a mixture of corticosteroid and anaesthetic is injected.
These are also known as cortisone injections or corticosteroid injections, and they aim to reduce inflammation around the site of the injection.
Glucocorticoids are produced naturally by your body to regulate inflammation. But sometimes, your body’s natural response isn’t enough to deal with ongoing inflammation.
This is when synthetic glucocorticoids (steroid injections) can be used to reduce inflammation. The injections reduce pain and swelling so you can return to moving normally.
Steroid injections for back pain are often recommended when conservative treatments like physiotherapy have not been successful. However, there can be long waiting lists for cortisone injections on the NHS, with 7.7 million people currently waiting for some type of NHS treatment [8]. Private treatment is usually a faster way to access steroid injections for SI joint pain.
Platelet Rich Plasma (PRP) injections
PRP injections are a type of regenerative medicine used to accelerate or stimulate your body’s natural healing process. With PRP, platelets are collected from your blood and concentrated into a sample.
The sample is then injected into the affected area. This releases growth factors that increase the number of reparative cells produced by your body, enhancing and speeding up the healing process. Research shows that PRP therapy significantly improves SI joint pain [9].
The SI joint is a complex region and accuracy is vital for effective injections. That’s why Harley Street Specialist Hospital offers ultrasound-guided steroid injections and PRP injections. This means ultrasound imaging is used to display the area that will be injected, which makes for significantly more accurate and effective injections than when imaging is not used [10].

Surgery
Surgery is considered when non-surgical treatments have not resolved your symptoms. Usually, you try these treatments for several months before resorting to surgery.
Sacroiliac joint fusion is the surgery used to address SI joint pain. It aims to stop all movement at the SI joint by joining your ilium (pelvis) and sacrum together.
Screws, rods and sometimes a bone graft are used to fuse the joint – previously, open surgery was used. However, modern procedures are minimally invasive, using only a small incision (cut) to access the joint. This improves recovery time, pain and function following the procedure [11].
Here is the process for minimally invasive SI joint fusion:
- You are placed under general anaesthetic – you will not be conscious or aware of the surgery.
- Your surgeon makes a small incision on your lower back and moves your muscles to the side.
- Your surgeon drills a small hole through your ilium to access the SI joint.
- Ligaments and muscles are cleared away from the joint.
- Surgical implants and a bone graft are placed across the joint to encourage it to fuse together.
- Your surgeon puts the muscles back in place and closes the incision with stitches.
Recovery and prevention of SI joint pain
If you’ve had treatment for SI joint pain, there are principles to follow to ensure your pain doesn’t return. It’s important to return to work and your daily activities as soon as you feel able, although you may need a phased return to work or light duties for a period of time.
Factors that improve recovery and help prevent recurrence of SI joint pain are:
- Regular exercise, including stretching and strengthening. You may continue with your physiotherapy exercises long-term to prevent your pain from returning.
- An ergonomic workstation
- Maintaining a healthy weight and good nutrition
- Lifting with proper lifting techniques – your physiotherapist can show you how to do this
- Avoiding smoking or excessive drinking
- Relaxation, mindfulness and stress management techniques
- Proper posture during standing, sitting and sleeping
During recovery, you may be given a pelvic brace to limit painful movements and stabilise your pelvis. Your surgeon will likely recommend physiotherapy, ice and pain medication.
Alternatives to NHS treatment for SI joint pain
If you’d prefer to access treatment at a time that suits you, private treatment could be right for you. Harley Street Specialist Hospital offers access to a specialist pain management unit, diagnostic imaging, private physiotherapy and world-renowned spinal and orthopaedic surgeons.
Book an appointment to arrange an expert assessment of your SI joint pain. Assessment and treatment can often take place on the same day.




