Bilateral sciatica is a condition that causes pain and altered sensation in your buttocks and legs. Sciatica occurs when your sciatic nerve is compressed or irritated. ‘Bilateral’ means that your symptoms are on both sides.
You may have a range of symptoms, from mild and irritating to severe and disabling. This is because there are many different reasons your sciatic nerve can become irritated, and it can be affected to different degrees. If you have pain in both legs and you’re not sure what’s causing it, Harley Street Specialist Hospital can help by providing a clear diagnosis and treatment plan.
Here, we’ll discuss why bilateral sciatica is a red flag, what causes your sciatic nerve to flare up, and how you can treat bilateral sciatica pain.
What causes the sciatic nerve to flare up?
There are several reasons that both branches of your sciatic nerve may flare up at the same time, resulting in bilateral sciatica. These range from common conditions like herniated discs to rare conditions like CES.
Herniated disc
Herniated discs are common, and every year 1-3% of people will experience a symptomatic herniated disc in their lower back [1]. A disc that herniates on both sides can compress both branches of the sciatic nerve, causing the symptoms of bilateral sciatica.
Spinal stenosis
Spinal stenosis describes the narrowing of your spinal canal (where nerves pass through), putting pressure on your spinal cord [2]. This narrowing is commonly found in older adults [3].
Cauda Equina Syndrome
This is where a bundle of nerves in the lower part of your spinal cord are compressed at the same time, causing a wide range of symptoms in your lower body. These symptoms can include sciatica in one leg or both legs.
Piriformis syndrome
The piriformis muscle is located deep in your buttock. Sometimes this muscle can compress the sciatic nerve, causing symptoms of sciatica. For some people, this can happen on both sides at the same time.
Other reasons
There are a whole host of other causes of sciatica. These include nerve damage, tumours, muscle spasms, and bone spurs (often found in people with arthritis). Tumours are a much less likely cause than muscle spasms or a herniated disc, so there’s no need to assume the worst. Sciatica in pregnancy is also relatively common.
Why is bilateral sciatica a red flag and how is it diagnosed?
Bilateral sciatica is a red flag symptom for Cauda Equina Syndrome (CES). In CES, the bundle of nerves at the bottom of your spine (called the Cauda Equina) becomes suddenly compressed. This severely affects sensation and movement in your lower body [4]. CES is a relatively rare condition, and common symptoms are lower back pain, sciatica, loss of movement and sensation of your lower body, and problems with your bowel and bladder.
Around 2.7 people per 100,000 are diagnosed with CES each year [5]. It’s most common in women aged 30-49 and of the people that present with CES symptoms, 19% are diagnosed with CES [5].
Although research shows that people with CES may also present with unilateral sciatica (on one side), outcomes tend to be worse for people with bilateral sciatica [4]. Around half of people with CES also have bilateral sciatica [6].
If you do have bilateral sciatica, it’s important to get advice from a healthcare professional as soon as possible. This is particularly important if you have any of these other symptoms of CES:
- Inability to pass urine or incontinence
- Bowel incontinence or problems with your bowel
- Tingling or numbness between your legs and around your buttocks (the ‘saddle’ region)
How do you treat bilateral sciatica pain?
There are a range of treatment options available for bilateral sciatica pain. The best treatment for you will depend on your symptoms, the cause of your pain and personal preference. Many cases of sciatica will go away on their own, but it’s a good idea to consider treatments that can help to speed up that process.
The first step is diagnostic imaging to determine where your pain is coming from. Imaging like X-rays and MRI scans are helpful to identify the source of your pain. Once you know the root cause of your pain, your doctor can recommend the best treatment.

Medication
Some medications can help to relieve bilateral sciatica pain. Ibuprofen, naproxen and other non-steroidal-anti-inflammatory drugs (NSAIDs) can provide temporary pain relief by reducing inflammation. Research into the use of NSAIDs for sciatica is limited, although NSAIDs have been shown to work better than a placebo [7].
It’s not a good idea for some people to take these medications, including people with medical conditions like chronic kidney disease [8]. It’s always wise to take them with food because they can irritate your stomach.
Whether you have other medical conditions or not, it’s worth speaking to your doctor before starting any new medications. Different people need to take medicines in different ways, so a chat with your doctor can reduce your risk of side effects.
Topical medication (applied to your skin) can be a good way to get fast relief from sciatica. These medicines can be faster to act because they start closer to the source of the pain. A few topical medications that can help bilateral sciatica [9] are:
- Menthol
- Camphor
- Capsaicin
- Cannabidiol (CBD)
- Methyl salicylate
- Lidocaine patches for extended pain relief
Both menthol and camphor have only a small pain-relieving effect, but they help to improve the skin penetration of other pain-relieving drugs like NSAIDs. Many topical pain-relief formulations contain both menthol and camphor alongside NSAIDs.
For severe cases of sciatica, your doctor may prescribe a muscle relaxant like diazepam. Sometimes your doctor may also prescribe steroids like prednisone for a short time, to help with inflammation around your spine.
Physiotherapy
Physiotherapy is often one of the first treatments recommended for sciatica. The goal of physiotherapy is to reduce pain and restore normal movement, strength, and function through exercise and pain-relieving techniques.
Unfortunately, NHS waiting lists can be very long for physiotherapy. That’s why many patients choose private care, such as Harley Street Specialist Hospital’s physiotherapy service, to improve their symptoms as soon as possible. Learn more about what the NHS can do for sciatica.
It’s always best to speak to a physiotherapist before starting a new exercise regime for sciatica. Different people need different exercises, and the exercises below won’t be suitable for everyone. Once you have a diagnosis, here are some of the exercises that your physiotherapist may teach you:
If your sciatica is very painful, a good time to do your physiotherapy exercises is after taking pain relief. This will allow you to move more freely, benefit more from the exercises and experience less pain while doing them.
Exercise
As well as specialist physiotherapy exercises, general exercise is often recommended too for sciatic pain. Some people find that gentle, low-impact exercise like yoga, Pilates or walking helps their symptoms.
Injections
If your sciatic pain hasn’t improved with time, physiotherapy or gentle exercise, you may be considering other treatments. Spinal injections are often the next step in treating sciatic pain. These deliver localised medication based on where your symptoms are coming from. Below, we’ve listed some of the most common types of injections for sciatic pain.
- Selective nerve root block – this can be useful to diagnose exactly where your pain is coming from. A steroid medication is injected into the root of a specific nerve and if your pain goes away, you’ve found the cause. You’ll also get temporary pain relief from this type of injection.
- Epidural steroid injection – this is a steroid injection designed to reduce inflammation around the nerve roots in your lower back. Reducing inflammation can take the pressure off an irritated nerve and improve your symptoms.
- Facet joint injections – these are steroid injections between the vertebrae in your spine. They can give you temporary pain relief to allow you to start moving normally again, which is often the precursor to recovery.
- Sacroiliac joint block – these are injections between your pelvic bones and your sacrum. This treatment is available on the NHS for individuals who suffer from sacroiliac joint pain. Sciatica can sometimes be caused by problems with your sacroiliac joint, and these injections can help your symptoms if this is the case.
- Medial branch block – this is another type of nerve block injection, where medication is injected into your medial nerves. These nerves are connected to the facet joints between the vertebrae of your spine.
- Lateral branch block – these injections are given to the nerves along the back of your sacrum. They can provide temporary relief and help to diagnose your pain.
- Radiofrequency ablation – a needle is inserted into your back, which delivers radio waves that create heat. This heat damages the nerves that are causing your pain and stops them from sending pain signals to your brain, so you don’t feel the pain any more.
- Regenerative injections – these help to stimulate and speed up your body’s natural healing process. One example is Platelet-Rich Plasma therapy (PRP). This is where platelets from your own blood are injected to speed up the healing of soft tissue that may be causing your sciatic pain. Another example is intradiscal stem cell injections – doctors use these to reduce pain and restore the function of the discs that separate the bones of your spine.
Harley Street Specialist Hospital offers steroid injections and nerve blocks as part of our pain management service. If you’d like an expert assessment to identify your treatment options, book an appointment at our London hospital.
Surgery
If you have tried several types of non-surgical treatment and your leg pain or weakness hasn’t resolved, surgery may be your next step. Usually, surgery isn’t considered until you have already tried other treatments. However, there are some scenarios where surgery may be considered immediately. These include:
- Severe fractures
- Tumours
- Cysts or abscesses
- Cauda Equina Syndrome
- Severe disc herniation
- Central spine stenosis
- Infection that isn’t responding to medication
The goal of surgery is to improve leg pain and weakness associated with sciatica and treat the root cause of it. However, if you also have back pain, this may or may not improve with surgery [10].
Microdiscectomy
If your bilateral sciatica is caused by a herniated disc in your lower back, one surgical option is microdiscectomy. In this type of surgery, the surgeon makes a small incision in your lower back and removes part of the disc or bone that’s compressing your nerve root.
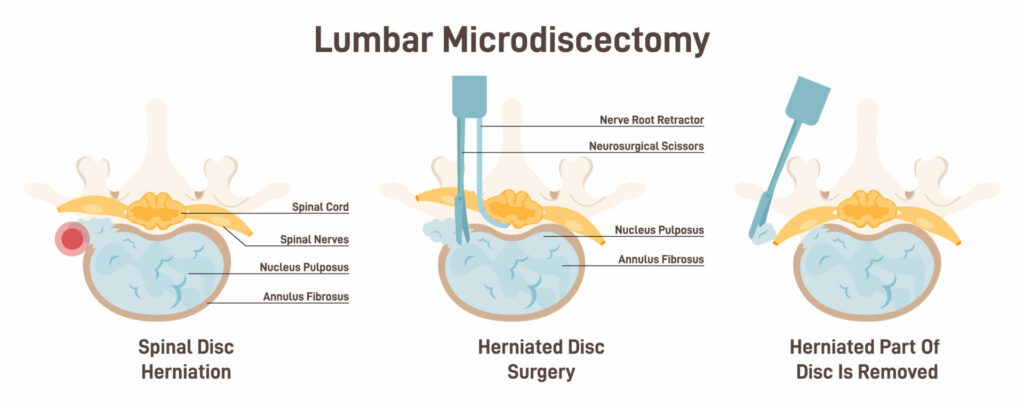
Because of the small incision, there is minimal damage to the tissue around the operation site. Research on microdiscectomies showed that around 4 years post-op, 84.3% of patients reported good or excellent results [11]. Some studies found this can be as high as 90% [12]. However, as with all surgeries, there is a risk that your symptoms could stay the same or worsen.
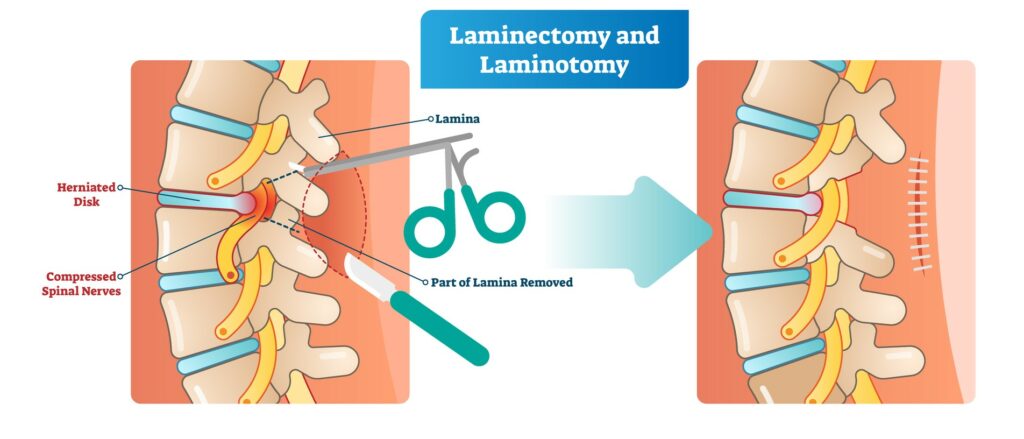
Lumbar decompression surgery
‘Lumbar’ refers to your lower back. Decompression surgery aims to take pressure off your sciatic nerve, treating the cause of your pain. There are several different types of lumbar decompression surgery:
- Laminectomy – this is where part of your lamina is removed, and is a common approach for people with spinal stenosis. Your lamina is what provides support and protection for the back of your spinal cord, but sometimes it can put pressure on your nerves. Removing the lamina creates more space for your nerves and can take the pressure off your sciatic nerve. Research shows this has a 75% long-term success rate [12].
- Foraminotomy – this is another type of surgery that creates more space for your nerve root. Bony growths (lumps of bone that grow in the spine when it has been damaged by arthritis) are surgically removed, enlarging your neuroforamen (where your spinal nerve exits the spine).
- Facetectomy – your facet joints connect the bones of your spine together, and your nerve roots pass through these joints. Over time, wear and tear of these joints can put pressure on your nerve roots, causing sciatica symptoms. In a facetectomy, the facet joints are trimmed or removed to relieve that pressure. Around 85% of people find this surgery relieves their pain [13].
Get the support you need for bilateral sciatica
It’s important to get bilateral sciatica assessed by a medical professional. Harley Street Specialist Hospital offers physiotherapy, an extensive pain management service and specialist spinal surgeons who can help.
If you have shooting pains in both legs, our expert team can help you find the best way forward. Book an appointment at our private London hospital for rapid assessment, diagnosis and treatment.




